Urinary Incontinence: How Thermiva® can help
What is urinary incontinence?
Urinary incontinence is when control over the urinary sphincter is either lost or weakened, causing involuntary leakage of urine. It’s a very common problem affecting both men and women.
According to the American Urological Association, one-quarter to one-third of men and women in the United States experience urinary incontinence – but it’s much more common for women. An estimated 30 percent of females aged 30-60 are thought to suffer from it, compared to 1.5-5 percent of men.
Quick Navigation

Fast facts on urinary incontinence
- Urinary incontinence is more common in females than in males.
- There are a number of reasons why urinary incontinence can occur.
- Obesity and smoking are both risk factors for urinary incontinence.
- It can be due to stress factors, such as coughing.
- It can happen during and after pregnancy.
- The chances of it happening increase with age.
- Bladder control and pelvic floor, or Kegel, exercises can sometimes help prevent or reduce it.
Causes & Types of Urinary Incontinence
The causes and the type of incontinence are closely linked.
Stress incontinence
Factors:
- pregnancy and childbirth
- menopause, as falling estrogen can make the muscles weaker
- hysterectomy and some other surgical procedures
- age
- obesity
Symptoms:
This is the most common kind of urinary incontinence, especially among women who have given birth or gone through the menopause.
In this case “stress” refers to physical pressure, rather than mental stress. When the bladder and muscles involved in urinary control are placed under sudden extra pressure, the person may urinate involuntarily.
The following actions may trigger stress incontinence:
- coughing, sneezing, or laughing
- heavy lifting
- exercise
Urge incontinence
Factors:
- cystitis, an inflammation of the lining of the bladder
- neurological conditions, such as multiple sclerosis (MS), stroke, and Parkinson’s disease
- enlarged prostate, which can cause the bladder to drop, and the urethra to become irritated
Symptoms:
Also known as reflex incontinence or “overactive bladder,” this is the second most common type of urinary incontinence. There is a sudden, involuntary contraction of the muscular wall of the bladder that causes an urge to urinate that cannot be stopped.
When the urge to urinate comes, the person has a very short time before the urine is released, regardless of what they try to do.
The urge to urinate may be caused by:
- a sudden change in position
- the sound of running water
- sex, especially during orgasm
Bladder muscles can activate involuntarily because of damage to the nerves of the bladder, the nervous system, or to the muscles themselves.
Overflow incontinence
Factors:
- an enlarged prostate gland
- a tumor pressing against the bladder
- urinary stones
- constipation
- urinary incontinence surgery which went too far
Symptoms:
This is more common in men with prostate gland problems, a damaged bladder, or a blocked urethra. An enlarged prostate gland can obstruct the bladder.
The bladder cannot hold as much urine as the body is making, or the bladder cannot empty completely, causing small amounts of urinary leakage.
Often, patients will need to urinate frequently, and they may experience “dribbling” or a constant dripping of urine from the urethra.
Total incontinence
Factors:
- an anatomical defect present from birth
- a spinal cord injury that impairs the nerve signals between the brain and the bladder
- a fistula, when a tube or channel develops between the bladder and a nearby area, usually the vagina
Symptoms:
This either means that the person leaks urine continuously, or has periodic uncontrollable leaking of large amounts of urine.
The patient may have a congenital problem (born with a defect), there may be an injury to the spinal cord or urinary system, or there may be a hole (fistula) between the bladder and, for example, the vagina.
Mixed incontinence
There will be symptoms of both stress and urge incontinence.

Other causes:
These include:
- some medications, especially some diuretics, antihypertensive drugs, sleeping tablets, sedatives, and muscle relaxants
- alcohol
- urinary tract infections (UTIs)
Diagnosis
Ways to diagnose urinary incontinence include:
- A bladder diary: The person records how much they drink, when urination occurs, how much urine is produced, and the number of episodes of incontinence.
- Physical exam: The doctor may examine the vagina and check the strength of the pelvic floor muscles. They may examine the rectum of a male patient, to determine whether the prostate gland is enlarged.
- Urinalysis: Tests are carried out for signs of infection and abnormalities.
- Blood test: This can assess kidney function.
- Postvoid residual (PVR) measurement: This assesses how much urine is left in the bladder after urinating.
- Pelvic ultrasound: Provides an image and may help detect any abnormalities.
- Stress test: The patient will be asked to apply sudden pressure while the doctor looks out for loss of urine.
- Urodynamic testing: This determines how much pressure the bladder and urinary sphincter muscle can withstand.
- Cystogram: An X-ray procedure provide an image of the bladder.
- Cystoscopy: A thin tube with a lens at the end is inserted into the urethra. The doctor can view any abnormalities in the urinary tract.
Treatment
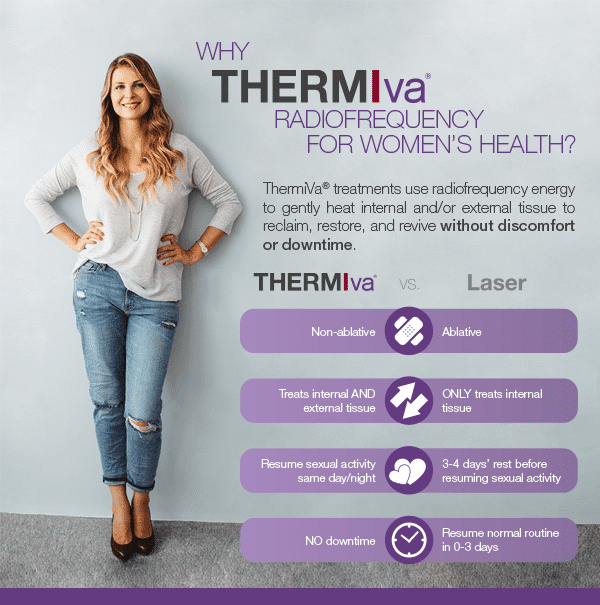
There are many different treatments for urinary incontinence – from “simple” Kegel exercises to surgery. We have found that Thermiva® is an amazing non-surgical option that treats all different types of UI.
Thermiva® uses radio frequency to heat up tissue in the lower urinary tract. When it heals it is often firmer, often resulting in better urinary control. Most patients describe the procedure as non-painful, just a slight “warming” sensation, and are able to go about their normal routines immediately afterwards.
Thermi-Va Pre-Treatment Recommendations
** Treatment is not recommended for pregnant women. **
- It is recommended to have a normal physical and pap smear within 2 years.
- If you have frequent urinary tract infections, please let our staff know.
- If you are prone to herpes outbreak, please let our staff know, as we may want to prescribe an anti-viral medication.
- Inform Dr. Janowski of any vaginal surgery or if you have been told you have any vaginal prolapse.
- We suggest increasing hydration one day prior to treatment. Drink an extra 4-6 glasses of water.
- We suggest emptying your bladder immediately before treatment.
- We recommend clipping or shaving the external treatment area at least one day prior to the procedure. (We recommend avoiding waxing or laser hair removal 5-7 days prior to avoid further irritation)
- Menstruating is not contraindicated. However, if you are in the middle of a heavy flow, you will want to reschedule for your own comfort.
- Cardiac devices such as AICD’s (auxiliary internal cardiac devices), defibrillators, mechanical valves, pacemakers, or any device that is affected by RF energy.
Treatment is NOT recommended if you have:
- Active sexually transmitted disease
- Current urinary tract infection
- Greater than a stage 2 pelvic organ prolapse
- Recent vaginal surgery or fillers may require an alternative treatment
TREATMENT SCHEDULE
Treatments are spaced approximately one month apart. A series of 3 treatments is recommended, with a “touch up” treatment done once per year thereafter.
Thermi-Va Post-Treatment Recommendations
- If treated externally, skin may be slightly pink to red, swollen and warm to the touch for approximately one to three hour(s) post procedure
- There is a possibility of some mild cramping, which should resolve in 24 hours
- There is a possibility of some light spotting immediately post procedure
- You may resume normal physical and sexual activity, unless otherwise directed by your provider
- You may experience some tenderness to the tissue immediately following treatment if you chose to engage in normal sexual activity.
- There are no restrictions on showering
- There are no restrictions on bathing, swimming or hot tubs (exception: if spotting or mild bleeding occur, wait one day to submerge the area in water)
Please call our office immediately (303-469-0064) if you have:
- Bleeding lasting longer than 24 hours
- Pain uncontrolled by over the counter-medication
- Cramping lasting longer than 24 hours
- A fever > 101 degrees.
*Results may vary from patient to patient
